

Neuroplasticity, the brain's ability to reorganize and form new neural connections, plays a crucial role in the brain's recovery from injury or trauma. Bioelectrical Signals Following an injury, the brain can rewire itself by forming new connections and pathways to compensate for the damaged areas. This process, known as neural reorganization, allows the brain to adapt and regain lost functions. Neuroplasticity enables the brain to relearn tasks and skills, contributing to the recovery process after injury or trauma. This adaptability is essential for rehabilitation and recovery, as it allows the brain to compensate for the areas that have been affected.
Neuroplasticity is fundamental to learning and memory formation. When new information is learned, the brain undergoes changes in its neural connections, forming and strengthening synapses. This process, known as synaptic plasticity, is essential for encoding and storing memories. Neuroplasticity enables the brain to adapt to new information and experiences, facilitating the formation of long-term memories and the acquisition of new skills. The brain's ability to reorganize and strengthen neural connections through neuroplasticity is crucial for learning and memory processes.
Brainwave FrequenciesNeuroplasticity can indeed be harnessed to improve rehabilitation outcomes for individuals with neurological conditions. By understanding the mechanisms of neuroplasticity, rehabilitation programs can be designed to promote the brain's adaptive capabilities. Techniques such as repetitive task training, sensory stimulation, and cognitive exercises can leverage neuroplasticity to enhance recovery and functional outcomes for individuals with neurological conditions. Harnessing neuroplasticity in rehabilitation can help optimize the brain's ability to reorganize and adapt, leading to improved recovery and quality of life for patients.

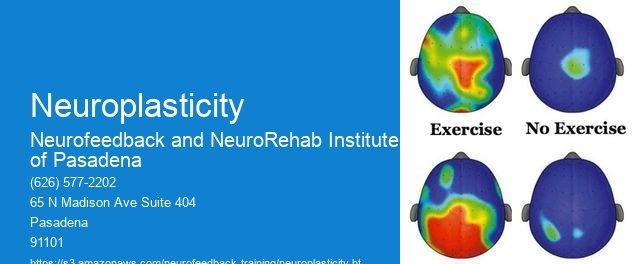
Aging can impact the brain's neuroplasticity and its ability to adapt to new experiences. As individuals age, the brain's neuroplasticity may decline, leading to reduced flexibility in forming new connections and adapting to changes. This can affect learning, memory, and the brain's ability to recover from injury or trauma. However, research suggests that certain lifestyle factors, such as physical exercise, cognitive stimulation, and social engagement, can support neuroplasticity in aging brains, potentially mitigating the impact of age-related changes on the brain's adaptive capabilities.
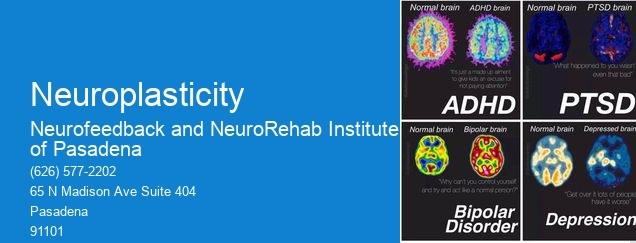
The potential implications of neuroplasticity in the treatment of mental health disorders are significant. Understanding how the brain can reorganize and adapt through neuroplasticity offers new avenues for developing interventions for mental health conditions. Epilepsy Monitoring Therapeutic approaches that target neuroplasticity, such as cognitive-behavioral therapy, mindfulness practices, and neurofeedback, aim to promote adaptive changes in the brain to alleviate symptoms of mental health disorders. By leveraging neuroplasticity, interventions can potentially facilitate the rewiring of maladaptive neural circuits, leading to improved mental health outcomes.
Different types of sensory input can influence neuroplasticity in the brain. Brainwave Synchronization Sensory experiences, such as visual, auditory, tactile, and olfactory stimuli, can induce changes in neural connections and synaptic strength. For example, sensory enrichment through exposure to diverse stimuli has been shown to promote neuroplasticity, enhancing learning and memory processes. Additionally, sensory deprivation or loss can impact neuroplasticity, highlighting the importance of sensory input in shaping the brain's adaptive capabilities. Understanding how sensory input influences neuroplasticity provides insights into how environmental factors can modulate brain function and plasticity.
Current research advancements in understanding the molecular mechanisms underlying neuroplasticity are shedding light on the intricate processes that drive the brain's adaptive capabilities. Neurofeedback Equipment Studies are uncovering the roles of various molecular and cellular processes, such as synaptic transmission, neurotrophic factors, gene expression, and epigenetic modifications, in shaping neuroplasticity. This knowledge is crucial for developing targeted interventions that can modulate neuroplasticity to promote recovery from injury, enhance learning and memory, and potentially address neurological and psychiatric conditions. Advancements in molecular neuroscience are paving the way for innovative approaches to harnessing neuroplasticity for therapeutic purposes.
Neurofeedback has been shown to have a positive impact on specific subcomponents of executive functioning, such as cognitive flexibility and inhibitory control. Studies have demonstrated that neurofeedback training can lead to improvements in cognitive flexibility, as evidenced by enhanced task-switching abilities and the ability to adapt to changing cognitive demands. Additionally, neurofeedback has been found to enhance inhibitory control, as indicated by improved impulse control and the ability to suppress irrelevant information. These improvements are thought to be mediated by the neuroplastic changes induced by neurofeedback, which can lead to enhanced connectivity and functioning within neural networks associated with executive functioning. Overall, neurofeedback appears to have a promising role in enhancing specific subcomponents of executive functioning, offering potential benefits for individuals seeking to improve cognitive flexibility and inhibitory control.
There have been several studies examining the long-term effects of alpha-theta neurofeedback for post-traumatic stress disorder (PTSD). Research has shown that alpha-theta neurofeedback can lead to significant reductions in PTSD symptoms, including anxiety, hyperarousal, and intrusive thoughts. Long-term follow-up studies have indicated that these improvements can be sustained over time, with some individuals experiencing continued benefits even after the neurofeedback sessions have ended. Additionally, studies have explored the neural mechanisms underlying the effects of alpha-theta neurofeedback on PTSD, shedding light on the potential neuroplastic changes that occur in the brain as a result of this intervention. Overall, the evidence suggests that alpha-theta neurofeedback may offer lasting therapeutic effects for individuals with PTSD.
The integration of real-time functional magnetic resonance imaging (fMRI) with neurofeedback has shown promising potential in the treatment of specific neurological and psychiatric disorders. By providing real-time feedback on brain activity, this approach allows individuals to learn to self-regulate their neural patterns, potentially leading to improvements in symptoms associated with conditions such as depression, anxiety, ADHD, and chronic pain. The use of neurofeedback in conjunction with fMRI enables clinicians to target specific brain regions and neural networks implicated in these disorders, offering a more personalized and targeted treatment approach. Furthermore, the real-time nature of fMRI neurofeedback allows for immediate adjustments and adaptations to the training protocol, enhancing its effectiveness in addressing individual variations in brain function and response to treatment. As research in this area continues to advance, the integration of real-time fMRI with neurofeedback holds promise for optimizing therapeutic interventions and improving outcomes for individuals with neurological and psychiatric conditions.
Yes, there are neurofeedback approaches that specifically target enhancing creativity in domains such as music composition and visual arts. These approaches often involve training the brain to increase alpha and theta brainwave activity, which are associated with relaxed, creative states of mind. Neurofeedback protocols may also focus on enhancing connectivity between brain regions involved in creative processes, such as the prefrontal cortex and the default mode network. By targeting these specific neural mechanisms, neurofeedback can help individuals cultivate and enhance their creative abilities in music composition, visual arts, and other creative domains.
Neurofeedback has shown promise in addressing specific cognitive deficits in individuals with various types of learning disabilities, extending beyond dyslexia. By targeting specific neural pathways and cognitive functions, neurofeedback can be tailored to address deficits related to attention, memory, executive function, and processing speed in individuals with learning disabilities such as dyscalculia, dysgraphia, and auditory processing disorder. This personalized approach allows for the customization of neurofeedback protocols to address the unique cognitive challenges associated with different types of learning disabilities, offering potential benefits in improving cognitive functioning and academic performance. Additionally, neurofeedback may also help individuals with learning disabilities develop better self-regulation and coping strategies, contributing to overall improvements in their learning and daily functioning.