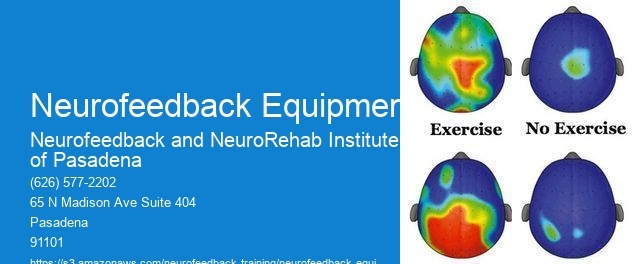
Neurofeedback equipment measures and monitors brainwave activity using electroencephalography (EEG) technology. EEG sensors are placed on the scalp to detect electrical activity in the brain. The equipment then amplifies and processes these signals to identify different brainwave frequencies, such as delta, theta, alpha, beta, and gamma waves. This data is displayed on a monitor, allowing clinicians to observe and analyze the brainwave patterns in real-time.
Specific types of brainwave frequencies that neurofeedback equipment targets for training include beta waves for focus and concentration, alpha waves for relaxation, theta waves for creativity and intuition, and delta waves for deep sleep and regeneration. By targeting these specific frequencies, neurofeedback equipment can help individuals learn to regulate their brainwave patterns and achieve desired mental states.
Neurofeedback Training ProgramNeurofeedback equipment can indeed be used to address specific neurological conditions such as ADHD or anxiety. Neurofeedback Through neurofeedback training, individuals can learn to self-regulate their brainwave patterns, leading to improvements in attention, impulse control, and emotional regulation. The equipment provides real-time feedback to the individual, rewarding desired brainwave patterns and helping to retrain the brain towards healthier functioning.

When selecting neurofeedback equipment for clinical use, key features to consider include the number and placement of EEG sensors, the quality of signal processing and analysis, the user interface for clinicians and patients, and the availability of customizable training protocols. Additionally, factors such as portability, ease of use, and compatibility with other clinical systems may also be important considerations.
Neurofeedback equipment differentiates between desired and undesired brainwave patterns during training sessions through a process known as operant conditioning. Neuromodulation When the individual's brain produces the desired brainwave patterns, they receive positive feedback, such as visual or auditory cues or rewards. Undesired brainwave patterns, on the other hand, result in the absence of feedback or a signal indicating the need for adjustment.
Typical training protocols and session durations recommended when using neurofeedback equipment can vary depending on the individual's needs and the specific condition being addressed. Bioelectrical Signals However, sessions typically range from 30 to 60 minutes, with multiple sessions per week recommended for optimal results. The training protocols are often tailored to the individual's specific goals and progress over time.
Specific safety considerations associated with the use of neurofeedback equipment include ensuring that the equipment is properly calibrated and maintained to provide accurate and reliable feedback. SMR (Sensorimotor Rhythm) Additionally, it's important to consider any contraindications, such as the presence of certain medical conditions or the use of medications that may affect brainwave activity. Clinicians should also be trained in the proper use of the equipment to ensure safe and effective neurofeedback training.

Neurofeedback has shown promise in targeting specific cognitive impairments in individuals with neurodegenerative diseases such as Alzheimer's or Parkinson's. By utilizing advanced brainwave monitoring techniques, neurofeedback can be tailored to address the unique cognitive challenges associated with these conditions. This personalized approach allows for the precise modulation of brain activity, potentially improving cognitive function, attention, and memory. Furthermore, neurofeedback interventions can be customized to address specific cognitive deficits, such as executive function, processing speed, and working memory, commonly affected in neurodegenerative diseases. The application of neurofeedback in this context represents a cutting-edge approach to addressing cognitive impairments in individuals with Alzheimer's or Parkinson's, offering a potential avenue for enhancing cognitive resilience and quality of life.
Neurofeedback has shown promising potential in enhancing specific facets of creativity, such as divergent thinking and idea generation. Research suggests that neurofeedback training can modulate brain activity, leading to improvements in cognitive flexibility, originality, and fluency of ideas. By targeting specific neural networks associated with creative thinking, neurofeedback may facilitate the generation of novel and unconventional ideas. Furthermore, the neuroplasticity-driven effects of neurofeedback could potentially enhance the brain's capacity for associative thinking, problem-solving, and insight generation. These findings underscore the potential of neurofeedback as a tool for augmenting various dimensions of creativity, offering new avenues for exploring its impact on cognitive processes related to idea generation and divergent thinking.
Neurofeedback has shown promise in targeting specific subtypes of schizophrenia symptoms, such as positive and negative symptoms. By utilizing electroencephalography (EEG) to measure brainwave activity, neurofeedback can be tailored to address the unique neural patterns associated with different symptom subtypes. For positive symptoms like hallucinations and delusions, neurofeedback may focus on regulating hyperactivity in specific brain regions, while for negative symptoms such as social withdrawal and apathy, it may aim to enhance connectivity and activity in areas associated with motivation and emotional processing. This personalized approach holds potential for addressing the diverse symptomatology of schizophrenia and improving overall treatment outcomes.
Neurofeedback protocols for treating depression in adolescents and adults may differ in terms of session duration, frequency, and specific neurofeedback techniques utilized. For adolescents, the protocols may need to be tailored to their developmental stage, considering factors such as brain plasticity and sensitivity to stimulation. Additionally, the emotional and cognitive aspects of depression in adolescents may require a more personalized approach, incorporating techniques that resonate with their age group, such as gamified or interactive neurofeedback. In contrast, neurofeedback protocols for adults may focus more on addressing long-standing patterns of depressive symptoms and may involve a more comprehensive assessment of cognitive and emotional functioning. The specific neurofeedback protocols for each group may also take into account the differences in brain development, hormonal influences, and social factors that can impact the manifestation of depression in adolescents versus adults.
There are potential contraindications for combining neurofeedback with certain pharmaceutical medications, particularly those that affect the central nervous system. It is important to consider the potential interactions between neurofeedback and medications such as antidepressants, anxiolytics, antipsychotics, and stimulants. Additionally, medications that influence neurotransmitter levels, such as serotonin, dopamine, and norepinephrine, may also have implications for neurofeedback treatment. It is advisable for individuals considering neurofeedback to consult with a healthcare professional, such as a psychiatrist or neurologist, to assess the potential risks and benefits of combining neurofeedback with specific pharmaceutical medications. This collaborative approach can help ensure the safety and efficacy of treatment while taking into account individual medical histories and current medication regimens.
Research on the use of neurofeedback for alleviating specific symptoms in individuals with traumatic brain injuries (TBI) has shown promising results. Studies have explored the efficacy of neurofeedback in addressing symptoms such as cognitive deficits, attention problems, emotional dysregulation, and motor impairments in TBI patients. Neurofeedback training has been found to modulate brain activity, enhance cognitive function, improve attention and concentration, regulate emotions, and enhance motor coordination in individuals with TBI. Furthermore, research has indicated that neurofeedback may contribute to neuroplasticity and promote recovery of brain function following TBI. These findings suggest that neurofeedback holds potential as a non-invasive and complementary intervention for addressing various symptoms associated with TBI. Further research is warranted to elucidate the specific mechanisms and optimal protocols for utilizing neurofeedback in TBI rehabilitation.
Yes, there are specialized neurofeedback protocols designed to address specific symptoms of obsessive-compulsive disorder (OCD). These protocols often focus on targeting the hyperactivity in the orbitofrontal cortex and the anterior cingulate cortex, which are areas of the brain associated with OCD symptoms such as intrusive thoughts, compulsive behaviors, and anxiety. Neurofeedback training for OCD may involve protocols that aim to regulate brainwave patterns, such as enhancing alpha and theta waves while reducing beta waves, to promote relaxation, reduce impulsivity, and improve cognitive flexibility. Additionally, specific neurofeedback protocols may also target enhancing connectivity between different brain regions, such as the prefrontal cortex and the striatum, to help regulate emotional responses and reduce the intensity of obsessive thoughts and compulsions. These specialized protocols are tailored to address the unique neurobiological underpinnings of OCD and can be an effective adjunctive treatment approach for managing the symptoms of the disorder.