In response to stress and anxiety, the brain engages in self-regulation processes to maintain a sense of balance and stability. This can involve the activation of the body's stress response system, including the release of hormones such as cortisol and adrenaline. The brain also modulates the activity of the amygdala, the hippocampus, and the prefrontal cortex to regulate emotional responses and cognitive functions. Additionally, the brain may initiate neuroplasticity mechanisms to adapt to stress and anxiety, reorganizing neural connections and pathways to cope with the challenges.
Neurotransmitters play a crucial role in the self-regulation of the brain in response to stress and anxiety. Brain Mapping For instance, serotonin, dopamine, and GABA are involved in regulating mood, emotions, and stress responses. These neurotransmitters help to modulate the activity of neural circuits involved in emotional processing and cognitive control. Imbalances in neurotransmitter levels can impact the brain's ability to self-regulate, potentially contributing to mood disorders and anxiety-related conditions.
Mindfulness and meditation techniques have been shown to have a positive impact on brain self-regulation. These practices can promote neuroplasticity, enhance emotional regulation, and improve attentional control. By engaging in mindfulness and meditation, individuals may strengthen the connectivity of brain regions involved in self-regulation, such as the prefrontal cortex and the insula. These techniques can also reduce the activity of the amygdala, which is associated with the processing of fear and stress.

Sleep plays a crucial role in the brain's ability to self-regulate. During sleep, the brain undergoes essential processes that contribute to emotional regulation, memory consolidation, and stress recovery. Adequate sleep supports the functioning of the prefrontal cortex, which is involved in decision-making and impulse control. Sleep deprivation, on the other hand, can impair the brain's self-regulation mechanisms, leading to increased emotional reactivity and decreased cognitive performance.
EEG (Electroencephalogram)Exercise influences the brain's self-regulation processes through various mechanisms. Physical activity can promote neurogenesis, enhance synaptic plasticity, and increase the production of neurotrophic factors, all of which contribute to improved cognitive function and emotional regulation. Exercise also stimulates the release of endorphins, which can modulate pain perception and mood. Additionally, regular exercise has been associated with reduced stress and anxiety levels, indicating its positive impact on brain self-regulation.
QEEG (Quantitative EEG)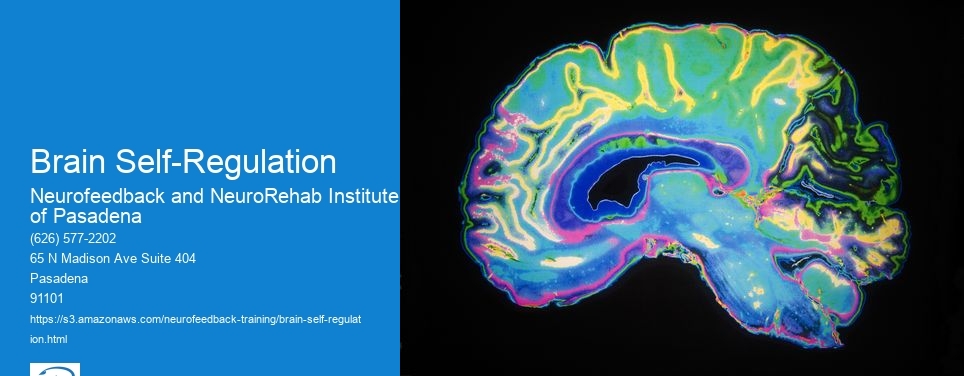
Nutrition and diet can significantly impact brain self-regulation. Consuming a balanced diet that includes essential nutrients such as omega-3 fatty acids, antioxidants, and vitamins can support brain health and function. SMR (Sensorimotor Rhythm) These nutrients play a role in neuroplasticity, neurotransmitter synthesis, and the regulation of inflammation, all of which are relevant to the brain's self-regulation processes. Conversely, poor dietary choices and nutrient deficiencies can compromise the brain's ability to self-regulate, potentially contributing to mood disturbances and cognitive impairments.
External factors, such as environment and social interactions, have a profound impact on the brain's self-regulation. A supportive and nurturing environment can promote resilience and emotional regulation, while exposure to chronic stressors or adverse experiences can disrupt self-regulation mechanisms. Social interactions and relationships also influence the brain's self-regulation, as they can provide emotional support, validation, and opportunities for regulation of emotions and stress. Positive social connections and a conducive environment can contribute to the development and maintenance of effective self-regulation skills in the brain.
Neurocognition
The anterior cingulate cortex (ACC) plays a crucial role in neurofeedback training by serving as a key brain region involved in regulating attention, emotion, and cognitive control. Through neurofeedback, individuals can learn to modulate the activity of the ACC, leading to improvements in self-regulation and emotional processing. This process involves real-time monitoring of brain activity, with the ACC as a focal point for feedback and training. By targeting the ACC, neurofeedback aims to enhance executive functions, reduce stress, and promote overall well-being. As individuals learn to self-regulate ACC activity, they may experience improvements in attention, emotional resilience, and cognitive flexibility, contributing to their overall mental and emotional health.
Yes, there are neurofeedback protocols specifically tailored to address language deficits in individuals with aphasia. These protocols often involve targeted training to enhance language processing, comprehension, and production. Neurofeedback techniques such as electroencephalography (EEG) and functional magnetic resonance imaging (fMRI) can be utilized to provide real-time feedback on brain activity related to language functions. By focusing on specific linguistic processes, such as phonological awareness, semantic retrieval, and syntactic processing, these protocols aim to retrain and optimize neural pathways associated with language skills. Additionally, incorporating tasks that stimulate language centers in the brain, such as word retrieval exercises and sentence construction activities, can further enhance the effectiveness of neurofeedback interventions for individuals with aphasia.
Neurofeedback has shown promise in enhancing specific motor skills in individuals with movement disorders such as Parkinson's disease. By utilizing real-time monitoring of brain activity and providing feedback to the individual, neurofeedback can help improve motor control, coordination, and balance. This approach can target specific brain regions and neural pathways involved in motor function, facilitating neuroplasticity and reorganization of neural networks. Additionally, neurofeedback can be tailored to address individual symptoms and challenges, offering personalized training to improve gait, fine motor skills, and overall movement abilities. Furthermore, the use of neurofeedback in conjunction with traditional therapies and medication may offer a comprehensive approach to managing motor symptoms in Parkinson's disease, potentially leading to improved quality of life for affected individuals.
Neurofeedback has shown promise as an adjunct therapy for managing specific neurological conditions such as epilepsy and migraines. By utilizing real-time monitoring of brainwave activity, neurofeedback aims to train the brain to regulate its own functioning, potentially reducing the frequency and severity of seizures in epilepsy patients and mitigating the intensity and frequency of migraines. This non-invasive technique involves providing feedback to the individual about their brainwave patterns, allowing them to learn self-regulation techniques. Research suggests that neurofeedback may help modulate cortical excitability and improve overall brain function, offering a potential complementary approach to traditional treatments for these neurological conditions. While further studies are needed to establish its efficacy, neurofeedback holds promise as a valuable adjunct therapy in the management of epilepsy and migraines.
Research has shown a growing interest in exploring the potential correlation between neurofeedback training and changes in the Default Mode Network (DMN). The DMN, a network of brain regions associated with self-referential thoughts and mind-wandering, has been the focus of studies investigating the effects of neurofeedback. Studies have suggested that neurofeedback training may lead to alterations in DMN connectivity, functional connectivity, and activity. These changes in the DMN have been linked to improvements in various cognitive and emotional functions. Furthermore, neurofeedback has been proposed as a potential tool for modulating DMN activity, potentially offering therapeutic benefits for conditions related to DMN dysfunction. However, further research is needed to fully understand the specific mechanisms and implications of the relationship between neurofeedback training and the DMN.