

Neurofeedback therapy targets and treats symptoms of ADHD in children by focusing on regulating specific brainwave patterns associated with attention and impulse control. Delta Waves By using neurofeedback, individuals can learn to self-regulate their brain activity, particularly in the theta and beta frequency bands. This training aims to enhance the brain's ability to maintain focus and inhibit impulsive behaviors, which are common challenges for children with ADHD. Through repeated sessions, neurofeedback helps retrain the brain to improve attention and self-control, leading to reduced ADHD symptoms and improved cognitive function.
In individuals with anxiety disorders, neurofeedback therapy aims to regulate specific brainwave patterns such as increased beta activity and decreased alpha and theta activity. By targeting these patterns, neurofeedback training seeks to promote a more balanced and relaxed state of mind, reducing excessive worry and fear. Through reinforcement of desired brainwave patterns, individuals can learn to self-regulate their brain activity, leading to decreased anxiety symptoms and improved emotional stability.
Neurofeedback training addresses symptoms of depression and improves mood regulation by targeting specific brainwave patterns associated with emotional processing and regulation. This therapy aims to regulate alpha asymmetry, frontal alpha power, and theta activity, which are often associated with depressive symptoms. Brainwave Frequencies By training individuals to modulate these brainwave patterns, neurofeedback helps promote a more balanced and stable emotional state, leading to improved mood regulation and reduced symptoms of depression.

Neurofeedback protocols used to enhance cognitive function and memory in individuals with traumatic brain injuries focus on regulating specific brainwave patterns such as alpha and beta activity. By targeting these patterns, neurofeedback training aims to improve cognitive processing, attention, and memory function. Brain-Computer Interface (BCI) Through repeated sessions, individuals can learn to self-regulate their brain activity, leading to enhanced cognitive function and improved memory recall.
Neurofeedback therapy helps individuals with insomnia by regulating their sleep patterns through targeting specific brainwave patterns such as alpha and theta activity. Neurological Disorders By training individuals to modulate these patterns, neurofeedback aims to promote a more balanced and relaxed state of mind, facilitating the transition into restful sleep. Through reinforcement of desired brainwave patterns, neurofeedback can help regulate sleep patterns and improve overall sleep quality for individuals struggling with insomnia.
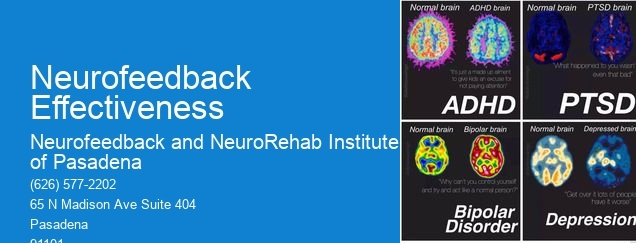
Specific neurofeedback techniques used to address symptoms of PTSD and improve emotional regulation focus on regulating brainwave patterns associated with hyperarousal and emotional dysregulation. Signal Processing By targeting specific patterns such as increased beta and theta activity, neurofeedback training aims to promote a more balanced and stable emotional state, reducing symptoms of hyperarousal and emotional reactivity. Through repeated sessions, individuals can learn to self-regulate their brain activity, leading to improved emotional regulation and reduced symptoms of PTSD.
Neurofeedback training targets and improves focus and attention in individuals with learning disabilities such as dyslexia by regulating specific brainwave patterns associated with attention and cognitive processing. By focusing on patterns such as increased theta and decreased beta activity, neurofeedback therapy aims to enhance the brain's ability to maintain focus and process information efficiently. Through reinforcement of desired brainwave patterns, neurofeedback can help improve focus and attention, leading to enhanced learning and cognitive function for individuals with dyslexia.
Neurofeedback has shown promising implications for addressing specific types of addiction, such as alcoholism and nicotine addiction. By utilizing neurofeedback techniques, individuals can potentially regulate their brain activity and improve self-regulation, which may contribute to reducing cravings and impulsive behaviors associated with addiction. This approach targets the brain's reward system, aiming to modify dysfunctional patterns and enhance cognitive control, ultimately aiding in the management of addictive behaviors. Additionally, neurofeedback may help individuals develop greater emotional regulation and resilience, potentially reducing the likelihood of relapse. The use of neurofeedback in addiction treatment aligns with the growing understanding of the neurobiological underpinnings of addictive behaviors, offering a potential adjunctive therapeutic approach to traditional interventions.
Neurofeedback training has shown promise in addressing specific symptoms of depersonalization/derealization disorders by targeting the dysregulated brainwave patterns associated with these conditions. By utilizing real-time monitoring and feedback, neurofeedback aims to modulate neural activity, promoting self-regulation and enhancing connectivity within the brain. This approach may help mitigate the dissociative experiences, emotional dysregulation, and cognitive impairments commonly observed in individuals with depersonalization/derealization disorders. Furthermore, neurofeedback training may contribute to improving self-awareness, emotional processing, and overall psychological well-being, offering a potential avenue for addressing the multifaceted nature of these conditions.
Neurofeedback training has been shown to modulate the specific connectivity patterns of the brain's default mode network (DMN) in meditation practitioners. Research indicates that neurofeedback can enhance the functional connectivity within the DMN, leading to improved self-awareness, attentional control, and emotional regulation. This modulation is thought to be mediated by the reinforcement of specific neural pathways associated with mindfulness and meditation practices. Furthermore, neurofeedback may facilitate the synchronization of neural oscillations within the DMN, promoting a state of relaxed alertness and heightened introspective awareness. These findings suggest that neurofeedback training holds promise for optimizing the connectivity patterns of the DMN in individuals engaged in meditation, potentially enhancing their overall mental well-being and cognitive performance.
Neurofeedback has shown promise in enhancing specific cognitive functions such as working memory. By utilizing real-time monitoring of brain activity and providing feedback to the individual, neurofeedback can target and train specific neural networks associated with working memory. This process involves reinforcing desired brainwave patterns and promoting neuroplasticity, which can lead to improvements in attention, focus, and information processing. Research suggests that neurofeedback may help individuals with attention-deficit/hyperactivity disorder (ADHD), traumatic brain injury, and other cognitive impairments to enhance their working memory capacity. Additionally, neurofeedback can be personalized to address individual cognitive needs, making it a potentially valuable tool for cognitive enhancement.
Yes, there are neurofeedback protocols specifically tailored to address different types of post-traumatic stress disorder (PTSD), including complex PTSD and combat-related PTSD. These protocols are designed to target the specific symptoms and underlying neural dysregulation associated with each type of PTSD. For example, protocols for complex PTSD may focus on addressing emotional dysregulation, dissociation, and interpersonal difficulties, while protocols for combat-related PTSD may target hyperarousal, hypervigilance, and re-experiencing traumatic memories. By utilizing neurofeedback techniques, such as alpha-theta training, SMR training, and coherence training, clinicians can customize treatment to address the unique neurophysiological patterns and symptoms of each type of PTSD, leading to more targeted and effective outcomes for individuals experiencing these specific forms of trauma-related stress.
The choice of neurofeedback modality, such as EEG, fNIRS, or qEEG, can significantly impact treatment outcomes for specific conditions. For instance, EEG neurofeedback is particularly effective in addressing conditions like ADHD, anxiety, and depression, as it allows for real-time monitoring and training of brainwave activity. On the other hand, fNIRS neurofeedback, with its ability to measure hemodynamic responses, may be more suitable for conditions related to cerebral blood flow and oxygenation, such as traumatic brain injury or stroke recovery. Additionally, qEEG neurofeedback, which involves quantitative analysis of EEG data, can offer personalized treatment approaches for conditions like epilepsy, insomnia, and cognitive impairment. The specific neurofeedback modality chosen should align with the targeted neural mechanisms and physiological processes associated with the particular condition being addressed, ultimately influencing the effectiveness of the treatment outcomes.
The anterior cingulate cortex (ACC) plays a crucial role in neurofeedback training by serving as a key brain region involved in regulating attention, emotion, and cognitive control. Through neurofeedback, individuals can learn to modulate the activity of the ACC, leading to improvements in self-regulation and emotional processing. This process involves real-time monitoring of brain activity, with the ACC as a focal point for feedback and training. By targeting the ACC, neurofeedback aims to enhance executive functions, reduce stress, and promote overall well-being. As individuals learn to self-regulate ACC activity, they may experience improvements in attention, emotional resilience, and cognitive flexibility, contributing to their overall mental and emotional health.