Outpatient therapy refers to a type of treatment where individuals receive therapy services on an outpatient basis, meaning they do not need to be admitted to a hospital or residential facility. This form of therapy allows individuals to receive treatment while still living at home and continuing with their daily activities. Outpatient therapy can be provided in various settings, such as clinics, private practices, or community mental health centers.
In contrast to inpatient therapy, outpatient therapy does not require individuals to stay overnight in a facility. Instead, they attend therapy sessions at scheduled times and then return home. This allows individuals to maintain their independence and continue with their regular routines. Inpatient therapy, on the other hand, involves individuals being admitted to a facility and receiving round-the-clock care and supervision.
Outpatient therapy can be used to treat a wide range of conditions and issues. It is commonly used for mental health concerns such as depression, anxiety, and substance abuse. It can also be beneficial for individuals recovering from physical injuries or surgeries, as well as those with chronic pain or illnesses. Additionally, outpatient therapy can address relationship issues, family conflicts, and provide support for individuals going through major life transitions.

The duration of outpatient therapy can vary depending on the individual's needs and the nature of their condition. Some individuals may only require a few sessions to address a specific issue, while others may benefit from ongoing therapy over a longer period of time. The therapist will work with the individual to develop a treatment plan that outlines the expected duration of therapy and the goals to be achieved.
Choosing outpatient therapy offers several benefits. Firstly, it allows individuals to receive treatment while still maintaining their daily routines and responsibilities. This can be particularly important for individuals who have work or family commitments. Additionally, outpatient therapy provides a more cost-effective option compared to inpatient therapy, as individuals do not incur the expenses associated with staying in a facility. Outpatient therapy also allows individuals to receive support from their community and loved ones, which can contribute to their overall well-being.

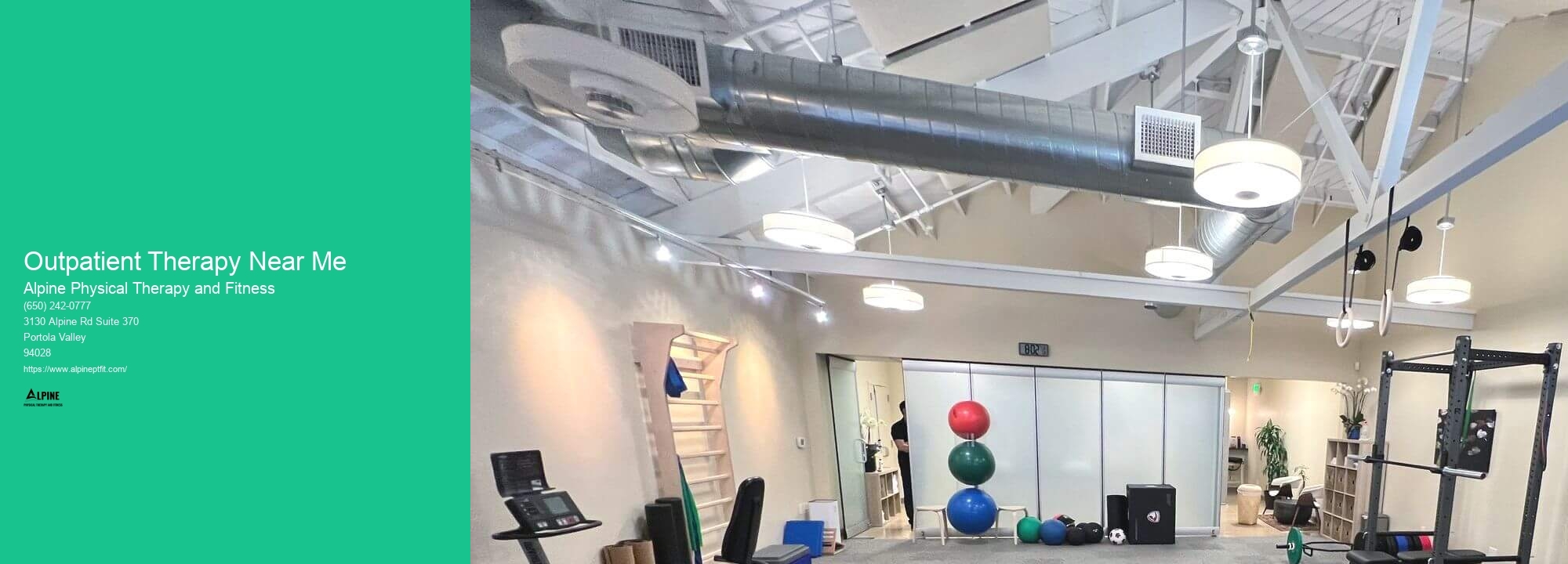
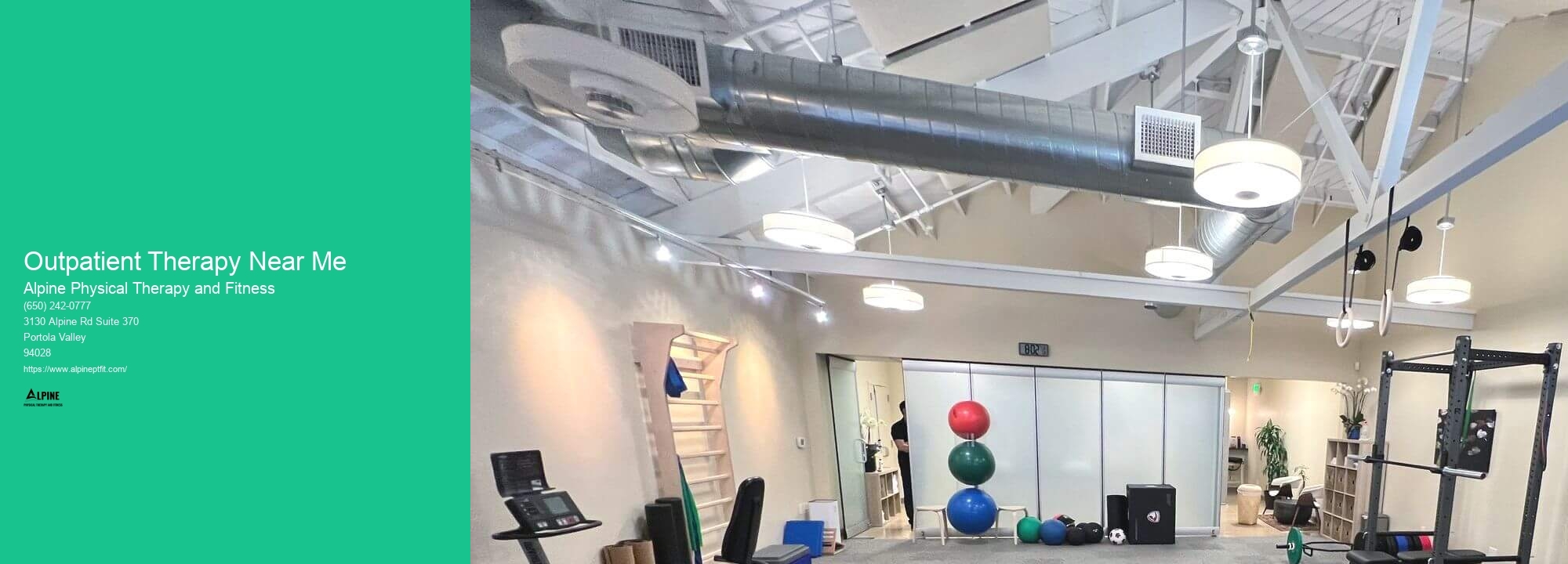
To find outpatient therapy near you, there are several resources available. You can start by contacting your insurance provider to inquire about therapists or clinics that are covered by your plan. You can also ask for recommendations from your primary care physician or seek referrals from friends, family, or trusted healthcare professionals. Online directories and search engines can also be helpful in finding therapists in your area.
During your first outpatient therapy session, you can expect the therapist to gather information about your background, medical history, and the reason for seeking therapy. They may ask you questions about your symptoms, emotions, and any previous treatment you have received. This initial session is an opportunity for the therapist to get to know you and understand your goals for therapy. It is also a chance for you to ask any questions or express any concerns you may have. The therapist will work with you to develop a treatment plan tailored to your specific needs and preferences.

The approach to treating individuals with hip impingement syndrome involves a comprehensive and multidisciplinary approach. The primary goal of treatment is to reduce pain, improve function, and prevent further damage to the hip joint. Non-surgical interventions such as physical therapy, activity modification, and anti-inflammatory medications are often the first line of treatment. Physical therapy focuses on strengthening the hip muscles, improving range of motion, and correcting any biomechanical abnormalities. In some cases, corticosteroid injections may be used to provide temporary pain relief. If conservative measures fail to alleviate symptoms, surgical intervention may be considered. Surgical options include arthroscopic procedures to remove or repair damaged tissue, as well as hip resurfacing or total hip replacement in severe cases. The choice of treatment depends on the severity of the impingement, the individual's age and activity level, and their overall health. A personalized treatment plan should be developed in collaboration with a team of healthcare professionals, including orthopedic surgeons, physical therapists, and pain management specialists, to ensure the best possible outcome for the individual.
Physical therapy plays a crucial role in improving the quality of life for patients with Parkinson's disease. By incorporating a range of specialized exercises and techniques, physical therapists can address the unique motor and movement challenges faced by individuals with Parkinson's. These exercises focus on improving balance, coordination, flexibility, and strength, which are often affected by the disease. Additionally, physical therapy can help manage symptoms such as rigidity, bradykinesia, and tremors, allowing patients to regain control over their movements. Through targeted interventions, physical therapy can also enhance gait and posture, reducing the risk of falls and improving overall mobility. Moreover, physical therapists provide education and guidance on adaptive strategies and assistive devices, empowering patients to navigate daily activities more independently. Overall, physical therapy offers a comprehensive approach to managing Parkinson's disease, promoting functional independence, and enhancing overall well-being.
Physical therapy can be highly beneficial in improving balance in individuals with multiple sclerosis. Multiple sclerosis is a chronic neurological condition that can lead to impaired balance and coordination. Physical therapists are trained to assess and address these specific issues through a variety of techniques and exercises. They may focus on improving core strength, flexibility, and proprioception, which are all crucial for maintaining balance. Additionally, physical therapists may use specialized equipment such as balance boards or stability balls to challenge and improve balance. By targeting these areas, physical therapy can help individuals with multiple sclerosis regain stability and reduce the risk of falls, ultimately enhancing their overall quality of life.
Physical therapists employ a variety of techniques to effectively treat common sports injuries such as sprained ankles. They typically begin by conducting a thorough assessment of the injury, taking into account factors such as the severity of the sprain, the individual's overall health, and any previous injuries. Treatment may involve a combination of manual therapy techniques, such as joint mobilization and soft tissue massage, to reduce pain and inflammation. Therapists may also utilize therapeutic exercises to improve strength, flexibility, and balance, helping to restore normal function and prevent future injuries. Additionally, modalities such as ultrasound or electrical stimulation may be used to further aid in the healing process. Education and guidance on proper body mechanics and injury prevention strategies are also integral components of a physical therapist's approach to treating sprained ankles.