Myofascial release is a therapeutic technique that focuses on releasing tension and tightness in the fascia, a connective tissue that surrounds and supports muscles, bones, and organs. It involves applying gentle pressure and stretching to the affected areas to help restore mobility and alleviate pain. The goal of myofascial release is to release restrictions in the fascia, which can become tight and restricted due to trauma, inflammation, or poor posture. By targeting these restrictions, myofascial release can help improve range of motion, reduce pain, and enhance overall physical function.
Myofascial release can be beneficial for a variety of conditions and issues. It is commonly used to treat chronic pain, such as back pain, neck pain, and headaches. It can also be helpful for conditions like fibromyalgia, temporomandibular joint disorder (TMJ), and sports injuries. Additionally, myofascial release can improve flexibility, posture, and athletic performance. It is often used as a complementary therapy alongside other treatments, such as physical therapy or chiropractic care.
While myofascial release can involve some discomfort, it is typically not considered painful. The pressure applied during a session is meant to be gentle and gradual, allowing the fascia to release tension without causing excessive pain. However, some individuals may experience temporary soreness or tenderness after a session, which is a normal response to the release of tension in the fascia. It is important to communicate with your therapist during the session to ensure that the pressure is within your comfort level.

The duration of a myofascial release session can vary depending on the individual and the specific needs of the treatment. On average, a session can last anywhere from 30 minutes to an hour. The therapist will assess your condition and develop a treatment plan that includes the appropriate duration for your sessions. It is important to note that multiple sessions may be necessary to achieve optimal results, especially for chronic conditions or long-standing issues.
The number of myofascial release sessions needed to see results can vary depending on the individual and the severity of the condition being treated. Some individuals may experience significant improvement after just a few sessions, while others may require more sessions to achieve their desired outcomes. Your therapist will work with you to develop a treatment plan that takes into account your specific needs and goals.

When performed by a trained professional, myofascial release is generally considered safe and does not have any significant side effects. However, it is important to communicate any concerns or medical conditions with your therapist before starting treatment. In rare cases, individuals may experience temporary bruising, swelling, or increased pain after a session. These side effects are typically mild and subside within a few days. It is also important to ensure that you are receiving myofascial release from a qualified and experienced therapist to minimize any potential risks.
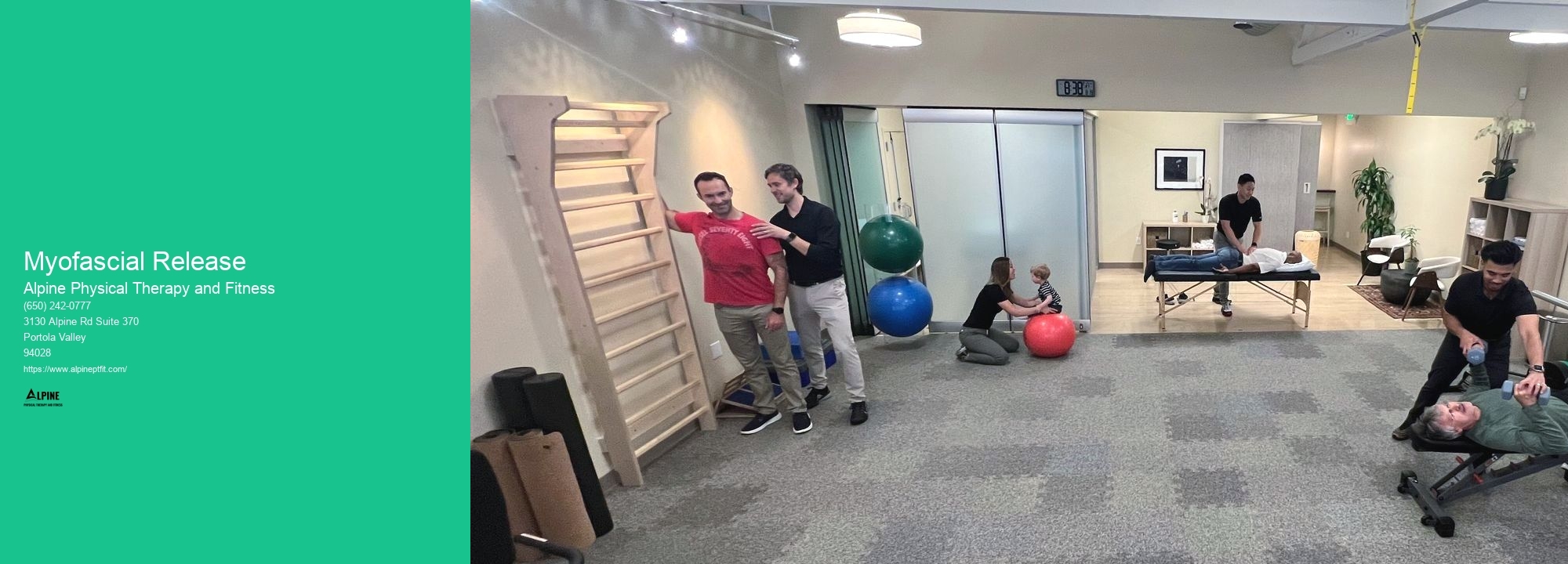
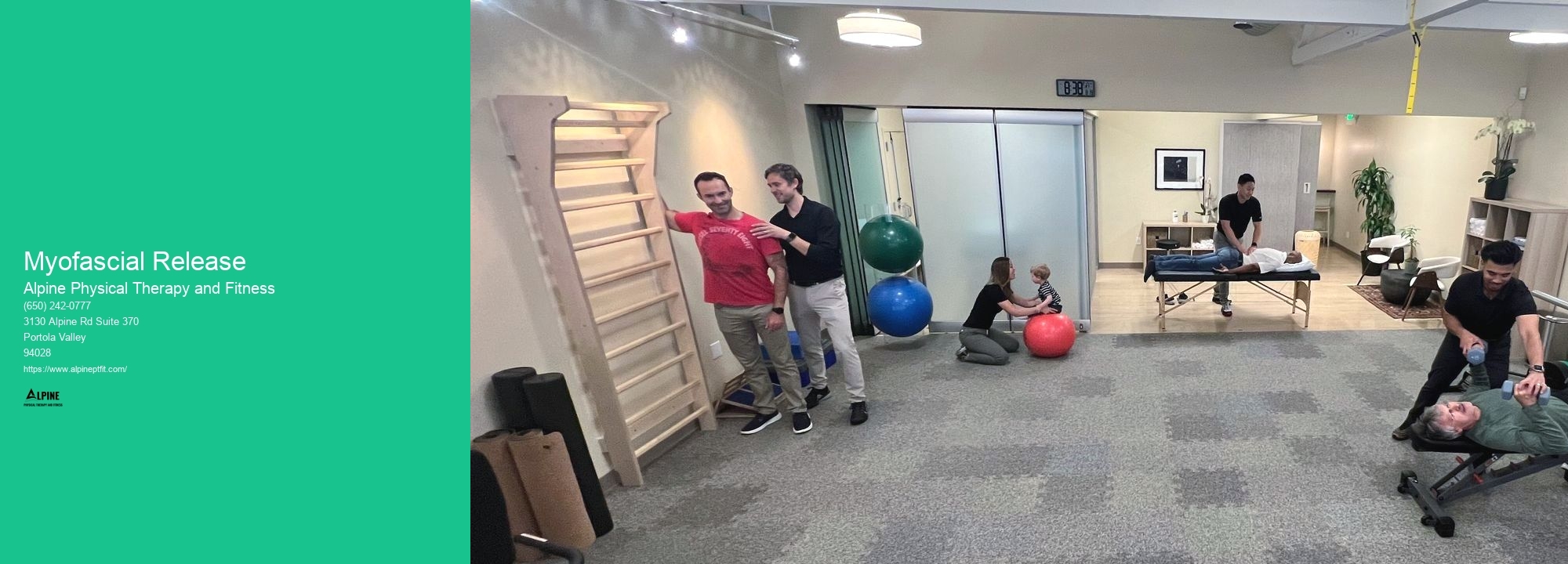
While it is possible to perform some myofascial release techniques at home using foam rollers or other tools, it is generally recommended to see a professional for a more targeted and effective treatment. A trained therapist has the knowledge and expertise to assess your condition, identify the areas of tension, and apply the appropriate techniques to release the fascia. They can also provide guidance on self-care exercises and stretches that can complement the in-office treatment. However, if you are unable to see a professional, there are resources available online that can guide you in performing basic myofascial release techniques at home.

Physical therapy plays a crucial role in assisting individuals with Guillain-Barré syndrome by promoting functional recovery and improving overall quality of life. Through a comprehensive rehabilitation program, physical therapists employ a variety of techniques and interventions to address the specific needs of each patient. These may include exercises to improve muscle strength, range of motion, and balance, as well as gait training to enhance mobility. Additionally, physical therapists may utilize modalities such as electrical stimulation and ultrasound to reduce pain and inflammation. By tailoring treatment plans to the unique challenges presented by Guillain-Barré syndrome, physical therapy helps individuals regain independence, restore physical function, and optimize their overall well-being.
Physical therapists employ a variety of techniques to address sacroiliac joint dysfunction. They begin by conducting a thorough assessment to determine the underlying cause of the dysfunction, which may include muscle imbalances, joint instability, or poor movement patterns. Based on their findings, they develop a personalized treatment plan that may include manual therapy techniques such as joint mobilizations, soft tissue mobilization, and myofascial release to restore proper joint alignment and improve mobility. They also prescribe specific exercises to strengthen the surrounding muscles and improve stability. Additionally, physical therapists may use modalities such as heat or ice therapy, electrical stimulation, or ultrasound to reduce pain and inflammation. Education on proper body mechanics and posture is also provided to prevent future episodes of sacroiliac joint dysfunction. Through a comprehensive and individualized approach, physical therapists aim to alleviate pain, improve function, and enhance the overall quality of life for individuals with sacroiliac joint dysfunction.
Plantar fasciitis is a common condition that causes pain and inflammation in the plantar fascia, a thick band of tissue that runs along the bottom of the foot. While there is no one-size-fits-all solution for alleviating plantar fasciitis pain, there are several exercises that can help. Stretching exercises, such as calf stretches and toe stretches, can help to loosen the plantar fascia and reduce pain. Strengthening exercises, such as toe curls and heel raises, can help to improve the stability and support of the foot. Additionally, exercises that focus on balance and proprioception, such as standing on one leg or using a balance board, can help to improve foot and ankle strength and stability. It is important to consult with a healthcare professional or physical therapist before starting any exercise program for plantar fasciitis, as they can provide personalized recommendations based on your specific needs and condition.
Breathing exercises are an integral part of pulmonary rehabilitation programs, as they help improve lung function and overall respiratory health. These exercises are typically incorporated into the program through a combination of education, guidance, and practice. Patients are taught various techniques, such as diaphragmatic breathing, pursed-lip breathing, and deep breathing exercises, which help strengthen the respiratory muscles and increase lung capacity. Additionally, patients may also be introduced to techniques like inspiratory muscle training, which involves using devices to provide resistance during inhalation, further enhancing respiratory muscle strength. The incorporation of breathing exercises in pulmonary rehabilitation programs aims to optimize lung function, reduce breathlessness, and improve overall quality of life for individuals with respiratory conditions.
The goals of physical therapy for children with cerebral palsy are to improve their motor skills, enhance their mobility, and promote their overall physical development. Physical therapists work closely with these children to address specific impairments such as muscle weakness, spasticity, and coordination difficulties. They employ a variety of techniques and interventions, including therapeutic exercises, stretching, and balance training, to help children with cerebral palsy gain better control over their movements and achieve greater independence in their daily activities. Additionally, physical therapy aims to prevent secondary complications, such as contractures and joint deformities, by promoting proper alignment and positioning. By focusing on these goals, physical therapy plays a crucial role in optimizing the functional abilities and quality of life for children with cerebral palsy.